ASU Biodesign Team explores radically new approach for developing viable lung tissue suitable for transplantation.
Lungs clothed in fresh cells offer new hope for transplant patients
For patients suffering 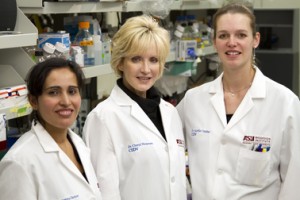 from severe pulmonary diseases including emphysema, lung cancer or fibrosis, transplantation of healthy lung tissue may offer the best chance for survival. The surgical procedure, however, faces two primary challenges: an acute shortage of donor lungs and rejection of transplanted tissue by the recipient’s immune system.
from severe pulmonary diseases including emphysema, lung cancer or fibrosis, transplantation of healthy lung tissue may offer the best chance for survival. The surgical procedure, however, faces two primary challenges: an acute shortage of donor lungs and rejection of transplanted tissue by the recipient’s immune system.
Now Daniel Weiss at the Vermont Lung Center (principal investigator for this project) in collaboration with Cheryl Nickerson and her colleagues at the Biodesign Institute at Arizona State University are exploring a radically new approach for developing viable lung tissue suitable for transplantation. The technique is being developed under a $3.4 million grant from the NIH to Weiss, $1.2 million of which is going to Nickerson for these studies. If successful, it could ultimately provide a virtually limitless supply of donor lung tissue while avoiding the host rejection that has long plagued organ transplantation.
While some biological structures (including bladder and skin) may be grown in the laboratory, building a complex organ like a lung from scratch is outside the realm of current medical technologies. The method under study instead involves audacious new techniques of tissue engineering. An organ extracted from a cadaver is chemically stripped of cells – a process known as decellularization – leaving behind a delicate architecture of the extracellular matrix. This scaffold is then recellularized – that is, repopulated using stem cells drawn from the intended transplant recipient.
Though they occur in all multicellular organisms, stem cells are exceptional biological entities. Different types of stem cells are being investigated in this study for the successful repopulation of the decellularized lung scaffolds. These cell types include pluripotent and multipotent stem cells. As their name implies, ‘pluripotent’ cells have the remarkable ability to form virtually any cell type in the body, including cardiac, muscle, neuron and the variety of cell types making up a functioning lung. Multipotent stem cells can give rise to a more limited number of lineages than pluripotent stem cells, but they are easier to obtain from patients and involve less downstream risks.
The working hypothesis of this study is that when stem cells are applied to the decellularized lung scaffolding, they take up residence throughout the structure, differentiating into the appropriate tissue and vasculature of a normal lung. It is believed that subtle chemical as well as mechanical forces direct this metamorphosis.
As Nickerson explains, this process of stem cell differentiation and rebuilding is assisted by placing the cells in a rotating wall bioreactor – a device that gently circulates fluid and oxygen through the cells in such a way as to mimic conditions during fetal development. Nickerson hypothesizes that the decellularized scaffolding subjected to this environment will help guide the stem cells adhering to this template to multiply and mature into the cell types essential for a functioning lung. Because the replacement organ is constructed with the recipient’s own cells, issues of immune rejection are minimal.
As the lungs under study are recellularized, they can be carefully evaluated in terms of biomechanics, vascular perfusion and normal lung phenotype, including the production of surfactants – lipoproteins essential for proper functioning of pulmonary alveoli. To accomplish the ambitious goals of the project, Nickerson and research assistant scientists in her laboratory, Aurélie Crabbé and Shameema Sarker, are part of a multidisciplinary team, which includes experts in lung biology, stem cells and regenerative medicine, thoracic surgery and bioengineering.
In addition to the NIH grant, work related to the lung recellularization project was honored as a recipient of the 2010 ASU/Mayo Clinic Seed Grant program. A review committee, made up of physicians and researchers from ASU and the Mayo Clinic, Phoenix, selected the work as one of the most outstanding grant proposals to be awarded funding. “Our end goal is to build new lungs from patient’s own cells, overcoming the need for donor organs,” says researcher Crabbé. “I am thrilled to be part of this exciting effort.”
In addition to her appointment at the Biodesign Institute, Cheryl Nickerson is a professor in the College of Liberal Arts and Sciences, School of Life Sciences.
