Researchers at Arizona State University’s Biodesign Institute explores an innovative means of investigating membrane proteins produced by a pair of highly pathogenic organisms. The research team showed that DNA-based genetic immunization, using a device known as a gene gun, could successfully express membrane proteins in mice and induce the animals to produce a range of critical antibodies to bacterial and viral targets.
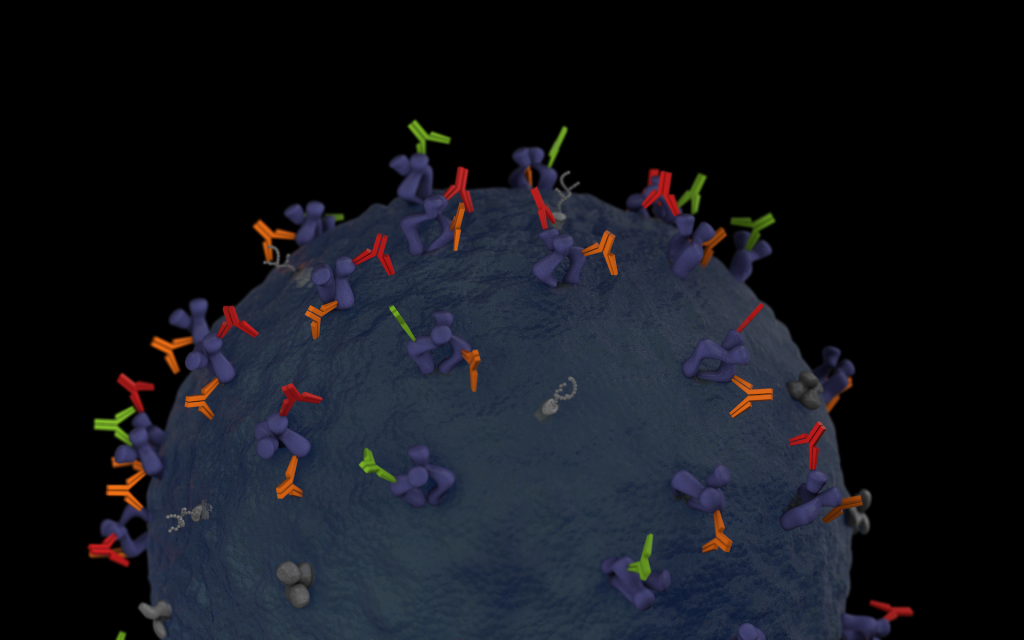
Antibodies, (seen in green, red and orange) bind with specific membrane proteins present on the cell surface. Graphic by Jason Drees for the Biodesign Institute.
In a new study, Debra Hansen, a research professor at Arizona State University’s Biodesign Institute, explores an innovative means of investigating membrane proteins produced by a pair of highly pathogenic organisms. The research team showed that DNA-based genetic immunization, using a device known as a gene gun, could successfully express membrane proteins in mice and induce the animals to produce a range of critical antibodies to bacterial and viral targets.

Debra Hansen is a research professor in the Center for Applied Structural Discovery at Arizona State University’s Biodesign Institute
“We learned that our new process of antibody production is incredibly efficient. If the membrane protein is naturally immunogenic, we easily generated high levels of antibodies using the genes alone,” Hansen says. “Rather than laboriously purifying the membrane protein and attempting to maintain the proper protein structure within detergents prior to immunization, we let the immunized host do the work for us.”
The new study also describes a method for expressing and purifying membrane proteins in a test tube and examining their binding activities with specific antibodies in blood extracted from gene immunized mice.
Conventionally, producing an immune response to a foreign protein requires purification of the protein, which is then injected into an animal. The process is cumbersome, challenging and time consuming. In the current study, an immune response is instead produced by directly introducing a gene encoding the protein of interest.
Two of the membrane proteins produced in the study were also successfully introduced into membranes of the bacterium E. coli, through the process of recombinant DNA. Use of the specific antibodies present in blood from gene-immunized mice demonstrated for the first time that both membrane proteins could be recombinantly expressed in a live organism, correctly fold into proper 3-D structures and migrate to the membranes within E. coli. These results now facilitate the structural determination of these two critical virulence proteins.
The research, which appears in the current issue of the Nature Publishing Group journalScientific Reports, promises to deliver new insights into the structure and function of membrane proteins of critical importance for medicine.
On the surface
Membrane proteins are implicated in innumerable functions in living organisms including cell signaling and communication, energy conversion and utilization, molecular transport and catalysis. Due to their involvement in a range of diseases, they have recently become primary targets for a new range of therapeutics. Indeed, more than 50 percent of all therapeutic targets are membrane proteins. The number is expected to rise as more is learned about membrane protein structure and function.
Despite their important role as the molecular interface in host/pathogen interactions as well as drug/cell relationships, membrane proteins account for less than 1 percent of the 100,000 unique protein structures presently catalogued. This is largely due to the serious challenges involved in producing, purifying, and determining the structures of membrane proteins. Hansen and her colleagues outline new strategies to produce antibodies–specialized proteins produced naturally by the immune system in response to pathogens or other threatening biological agents.
In the current study, they describe the use of a gene gun to introduce DNA information into a mouse. The handheld device uses a burst of gas to propel gold particles impregnated with circular DNAs known as plasmids into the skin in mice. The gold particles are known as micronanoplexes. The gene gun technology was pioneered and developed by Stephen A. Johnston, co-director of the Biodesign Center for Innovations in Medicine.
The genetic material introduced via the gene gun is taken up by mouse dendritic cells and translated into membrane protein in dermal tissues and lymph nodes. The mouse immune system responds by producing specific antibodies capable of binding to the membrane proteins. While the basic technique of genetic immunization has been in use for some time, the study marks the first description of the broad applicability of this approach to membrane proteins, as well as the first application of DNA-gold micronanoplexes to stimulate antibody production.
Bacterial and viral menaces examined
Results showed that genetic immunization successfully produced antibodies specific to 12 out of 17 membrane proteins from two Biosafety Level 3 pathogens: Francisella tularensis and African swine fever virus (ASFV). F. tularensis causes the disease tularemia. It is a widely studied infectious pathogen notorious for its ability to invade numerous cell types and cleverly evade the immune system. It is one of the most pathogenic bacteria on earth, capable of causing a fatal infection with as few as 10 cells. African swine fever virus is carried by arthropods. Infection in pigs causes a lethal and untreatable hemorrhagic disease that has devastated swine populations in areas of Africa and Eastern Europe.
Investigations of endogenous disease proteins produced by these organisms are difficult, requiring specialized safety facilities and protocols due to the potential danger they pose to researchers. The new method described permits the production of these pathogens’ membrane proteins and associated antibodies through DNA-based approaches, permitting the safe handling of biological material without risk of infection.
Once antibodies to specific membrane proteins have been produced in the mouse, the group sought to characterize the resulting mouse blood or sera. To do this, a new system known as in vitro translation in the presence of hydrophobic magnetic beads (IVT-HMB) was developed. Here, a small quality of membrane protein is produced in a test tube, simultaneously extracted using hydrophobic beads, then screened against the sera extracted from gene-immunized mice. Detection of a resulting signal in two types of diagnostic tests or assays (ELISA and Western blot) established the presence in the mouse sera of antibodies specific to each membrane protein. The IVT-HMB method represents a powerful streamlining of the production of membrane proteins, precluding the arduous process of isolation and purification traditionally required.
Stepping-stone to protein structures
Using X-rays to image tiny crystals of proteins is a powerful method to determine detailed protein structure, but the technique faces many challenges, including the difficulty of producing and purifying proteins that assemble properly. The current research marks a starting point for further structural characterization of membrane proteins, using such techniques as cryo-EM and X-ray crystallography.
Petra Fromme, a co-author of the new study and director of the Biodesign Institute’s Center for Applied Structural Discovery, highlights the power of the new research: “The range of antibodies produced through techniques like genetic immunization opens the door to high resolution molecular images of important membrane proteins,” she says. “The resulting antibodies assist structural determination in a variety of important ways, identifying properly assembled proteins, helping to induce proteins to assemble with other proteins into well ordered crystals and stabilizing or trapping proteins in active states that can be imaged using X-rays.”
In the next phase of research, the group plans to produce monoclonal antibodies using the same immunization process. These are essential as co-crystallization binding factors or ligands, used for the structural determination of membrane proteins via X-ray crystallography. The authors further note that the monoclonal antibodies produced through genetic immunization techniques offer attractive candidates for future therapeutics against a broad range of diseases.
This study was a combined effort of faculty in the Biodesign Institute, including Debra Hansen from the Center for Innovations in Medicine (CIM), Center for Applied Structural Discovery (CASD) and the School of Molecular Sciences (SMS), Kathryn Sykes from CIM and Petra Fromme from CASD and SMS, along with their teams of researchers and students, including: research scientists Mark Robida, Andrey Loskutov and Tien Olson, researchers Felicia Craciunescu, John-Charles Rodenberry and Hetal Patel and graduate student Xiao Wang from CIM and postdoc Katerina Dörner from SMS.
All of the necessary clones (plasmid DNAs) for applying this approach are available through the DNASU Plasmid Repository, which is housed in Biodesign’s Center for Personalized Diagnostics.
###
This work was funded by the NIH (NIGMS) under the PSI:Biology program, as part of the MPID (Membrane Proteins in Infectious Diseases) U54 grant, directed by Petra Fromme.
