Arizona Telemedicine Program is a Model ‘Telehealth Technology Innovation Accelerator’ for the Telemedicine Industry: A number of outstanding telemedicine programs, owned by different health-care organizations, work together on telemedicine challenges ranging from legal and regulatory issues, to telecommunications technology, to reimbursement.
Contact: AHSC Office of Public Affairs, 520-626-7301 Dec. 19, 2013
TUCSON, Ariz. – Investments by state governments in their own state universities can yield large returns and help create new industries. In Arizona, telemedicine is a good example of a success story.
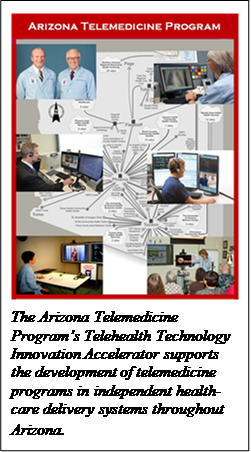
The Arizona Telemedicine Program’s Telehealth Technology Innovation Accelerator (TTIA) supports the development of telemedicine programs in independent health-care delivery systems throughout Arizona. The Arizona Telemedicine Program (ATP) operates one of the largest broadband health-care telemedicine service networks in the United States, delivers federally funded distance education and training programs throughout the Southwest and supports clinical studies on innovative health-care delivery systems.
Headquartered at the University of Arizona College of Medicine – Tucson, the ATP began in 1996, when then-State Representatives Robert “Bob” Burns (R-Glendale) and Lou Ann Preble (R-Tucson) championed the creation of an eight-site telemedicine program. Ronald S. Weinstein, MD, a pioneer in telemedicine and telepathology, was recruited as its founding director. Since then, the eight-site Arizona Telemedicine Rural Network has grown 20-fold, and now extends to 160 sites in 70 communities.
“Our goal from the start was to use state funding as seed money for something far greater,” said Dr. Weinstein. “Our University of Arizona physician faculty members and basic scientists saw an opportunity to create a new type of federation of telemedicine programs, in which the UA would have multiple roles for an Arizona state-wide consortium of telemedicine programs. These roles now include creating and operating a shared broadband telecommunications network; developing inclusive training programs that address the telemedicine training needs of personnel across the entire health-care industry in Arizona; and promoting telemedicine, telehealth and mobile health (or mHealth).”
Today, a number of nationally recognized telemedicine programs are affiliated with ATP. Personnel in these programs have received telemedicine training and technical assistance from ATP in Tucson and Phoenix or online.
The Yuma Regional Medical Center (YRMC) in Yuma, Ariz., signed on with ATP in 2006. Greg Warda, MD, and his YRMC staff now have daily access to pediatric cardiologists led by Daniela Lax, MD, at The University of Arizona Health Network (UAHN) in Tucson. Doctors in YRMC’s 20-bassinet Neonatal Intensive Care Unit have immediate access to UA telecardiologists in Tucson over the Arizona Rural Telemedicine Network. Immediate medical decisions can be made about transferring babies born with life-threatening congenital heart defects to Tucson or Phoenix hospitals with world-class pediatric cardiothoracic surgery specialists on their staffs. Said Dr. Warda, “I can’t say enough about the cardiologists in Tucson. They’ve all been wonderful.”
Each week, the UAHN cardiology group consults on four to five YRMC cases by telemedicine video conferencing and UA cardiologists also spend a day and a half each month in Yuma following up on the babies and children they have diagnosed. ATP engineers are available 24/7 to provide technical support for this pediatric service, which has handled more than 400 expedited cases in the past five years.
Another innovative program—Phoenix-based Banner Health’s eICU (electronic intensive care unit) program, one of the largest in the nation—utilizes clinical decision support systems (CDSS), computerized diagnostic aids that automate continual analysis of patient vital signs and provide electronic access to electronic health records, lab results, medications, medical imaging and other patient data. The CDSS alerts care teams to adverse trends as well as to acute events. Spotting adverse trends in a patient’s status is challenging in any care environment due to factors such as caring for multiple patients simultaneously and routine shift changes, but is critical to preventing adverse outcomes. The CDSS allows remote intensivists (physicians who specialize in the care and treatment of patients in intensive care units) and bedside care teams to focus their efforts on the patients who need them the most.
Banner’s eICU enterprise is built around a CDSS developed by faculty in the Department of Anesthesia at Johns Hopkins School of Medicine in Baltimore, Md., and is led by Deborah Dahl, vice president for patient care innovation and director of telemedicine at Banner. Currently, 430 eICU rooms at 20 Banner hospitals are equipped with a fixed two-way audio-video system linked to a call center in Mesa, Ariz., from which intensivists remotely monitor patients. In addition to providing the Banner Health “teleteam” video access, the system continuously gathers data from the bedside monitors and each patient’s electronic medical record. A single intensivist can follow hundreds of patients a day by telemedicine. The eICU system saves Banner Health tens of millions of dollars a year. It improves patient care, results in discharging patients earlier and lowers 30-day readmission rates.
Another ATP teaching affiliate, the Mayo Clinic in Phoenix/Scottsdale, has a network of rural telestroke sites. Bart M. Demaerschalk, MD, professor of neurology and director of the telestroke and teleneurology programs at the Mayo Clinic, and Ben Bobrow, MD, professor of emergency medicine at the UA College of Medicine – Phoenix created a state-wide rural telestroke and teleneurology program that serves 1,500 patients annually, preventing permanent brain damage and death. Their telestroke network is bringing “golden hour” diagnostic services to patients at Bisbee’s Copper Queen Community Hospital and other rural hospitals in Casa Grande, Cottonwood, Flagstaff, Globe, Kingman, Parker, Show Low, Tuba City and Yuma. (The “Golden Hour” for neurology patients is the one-to-three hours after stroke symptoms first appear, when the majority of strokes may be averted by intravenous thrombolytic therapy.)
The “granddaddy” of telemedicine services in Arizona is teleradiology, the most commonly used telemedicine application in the United States. Faculty in the UA Department of Medical Imaging (formerly Department of Radiology) pioneered the development of digital radiology, the foundational technology for teleradiology. Today, teleradiology services like those developed at the UA a decade ago are offered by hundreds of teleradiology companies in the United States. Since 1998, UA radiologists have diagnosed more than 1.3 million radiology cases for patients in 25 communities in Arizona and adjacent states.
“Today a number of our outstanding telemedicine programs, owned by different health-care organizations, work together on telemedicine challenges ranging from legal and regulatory issues to telecommunications challenges to reimbursement issues of mutual concern,” said Dr. Weinstein. The ATP is proud of the fact that “the Arizona State Legislature had a strong sense of ownership of the ATP at the time of its creation 17 years ago, and is engaged in these activities of ATP more than ever today.”
Dr. Weinstein noted, “Telemedicine is everybody’s business.”